Cutting-edge biopolymer 3D-printed heart valve technology to be commercialised in Australia to help millions globally suffering from aortic stenosis.
CUREator, Australia’s national biotech incubator, funds Western Australian biomedical engineering and medical research team to develop next-generation artificial heart valves through Medical Research Future Fund preclinical stream.
Fast Facts
- Aortic stenosis is a dangerous narrowing of the valve in the aorta blood vessel, reducing blood flow to the body and increasing pressure on the heart.
- Each year 9 million people worldwide suffer from aortic stenotic disease, which can be fatal without valve replacement.
- Around 1 in 8 elderly Australians has aortic stenosis.
- Current biological heart valves developed from animals can fail within 5 years.
- WA company CoraMetix Pty Ltd to develop 3D printed heart valve scaffold that mimics the mechanical properties of human valves with the aim to last the rest of the patient’s life.
Senior lecturer in biomedical engineering Dr Elena Juan Pardo at The University of Western Australia (UWA) and the Harry Perkins Institute of Medical Research has been selected to join Australia’s national biotech incubator – CUREator, which will assist in commercialising the cutting-edge heart valve technology.
The commercial acceleration incubator that specialises in medical innovation products is funded by the federal government’s Medical Research Future Fund (MRFF) administered by Brandon BioCatalyst. The incubator is designed to take promising medtech discoveries through early development to commercialisation.
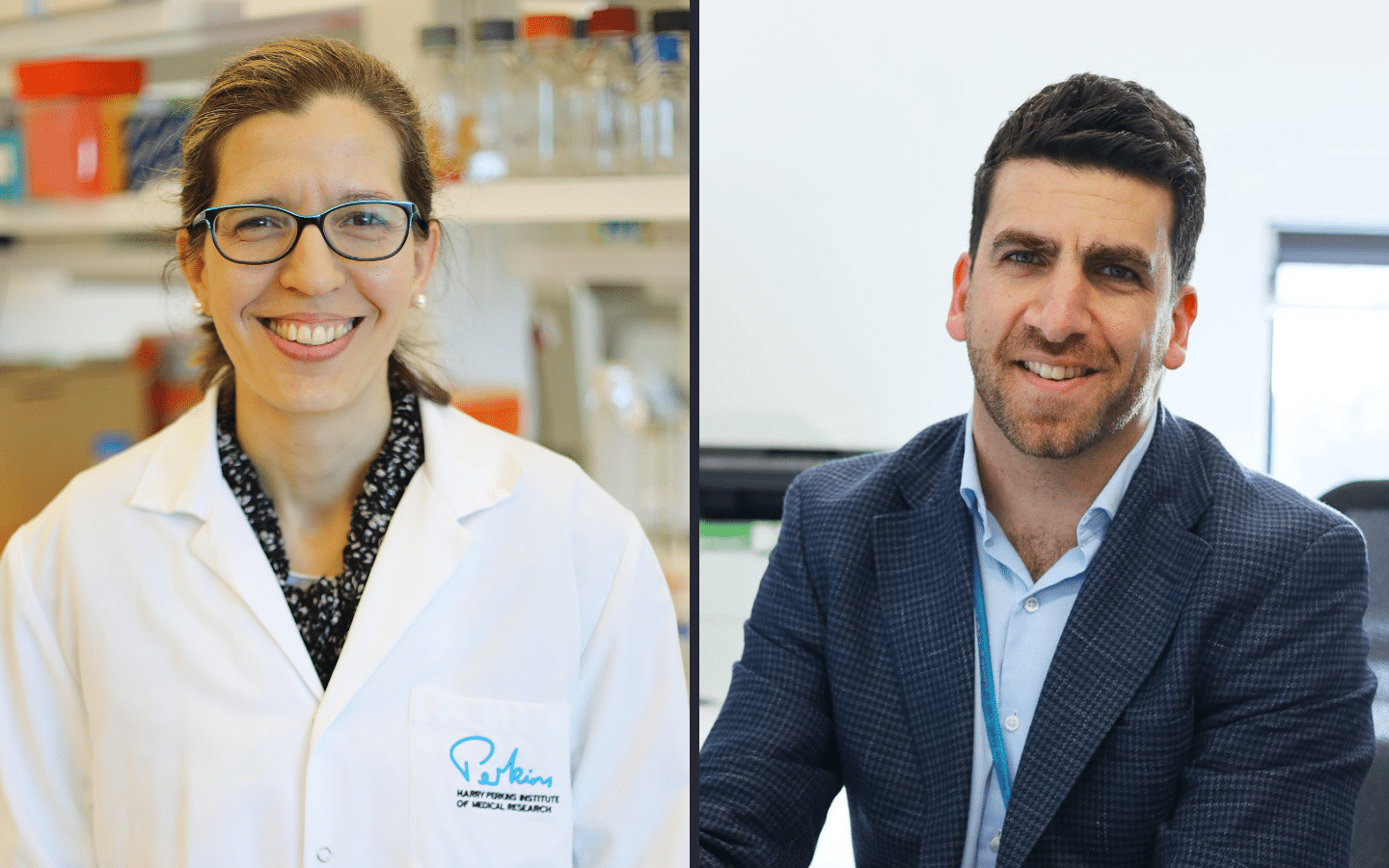
Newly formed Western Australian company, CoraMetix Pty Ltd, which will develop the new heart valves, will be led by Dr Juan Pardo (pictured above, left), alongside cardiologist and expert in the field of heart valve intervention and innovation, Dr Abdul Ihdayhid (pictured above, right), also affiliated with the Harry Perkins Institute of Medical Research.
Dr Juan Pardo (centre) with PhD Students Christopher Lamb (L) and Michael Vernon (R) with their 3D Printer in the T3mPLATE lab.
Dr Juan Pardo, who led the research team at UWA and the Harry Perkins Institute of Medical Research, said the $500,000 commercialisation accelerator grant was an integral phase on the path to testing the concept of biopolymer-based 3D-printed valves as a viable alternative to currently available animal-derived or carbon-fibre mechanical valves.
“Using a 3D-printing technique called Melt Electrowriting (MEW), we have designed and tested a patented biopolymer 3D-printed heart valve scaffold which exquisitely and uniquely mimics the mechanical properties of native human valves,” Dr Juan Pardo said.
Aortic stenosis, or a narrowing of the aortic valve opening, restricts the blood flow from the left ventricle to the aorta, leading to increased angina and breathlessness. Dr Ihdayid said that if left untreated, severe aortic stenosis can lead to heart failure and up to 50% patients not surviving beyond 2-3 years.
“With aging populations and better general health screening, more patients are being diagnosed. And as less invasive surgical techniques like transcatheter aortic valve replacement (TAVR) become more widely available, we’re seeing an increase in younger patients requiring intervention and therefore the issue of valve durability becomes even more crucial,” Dr Ihdayid said.
Most valve replacements today rely on biological valves derived from animal tissue, however these have a limited lifespan and can begin to fail within 5 years. This exposes patients to the need for repeat high-risk valve surgery or even some cases being deemed inoperable.
Dr Juan Pardo said, “Our 3D-printed solution will be cheaper to manufacture and require less ongoing medical intervention for the rest of the patient’s life. Most importantly, we are designing a valve to remain functional for the rest of the patient’s life, negating the need for repeat surgeries.
“Our team of international experts in biomedical engineering and cardiology aim to deliver a next-generation heart valve that provides best-in-class performance and durability.”
Trials in the US have suggested that untreated aortic stenosis could have a higher mortality rate than most common cancers.
Dr Juan Pardo continued, “As a biomedical engineer, I’m excited to be part of a collaborative team that is on the threshold of a new treatment option for such a serious disease.
“Our 3D-printed heart valve could change the lives of so many people, not only here in Australia, but around the world.
This CUREator grant means that we can continue our work here in Western Australia, to test our invention further, and bring it closer to realisation, and to the patients who need it most,” she said.
The global market for TAVR is estimated to grow from $4.4 billion USD is 2021 to around $13.4 billion USD by 2030.
