Breakthrough diagnostic technology to be commercialised in Australia in race to save millions globally from antibiotic resistant sepsis.
CUREator funds Western Australian research team to develop life-saving technology through the incubator’s CSIRO funded health security stream.
Fast Facts
- Each year 1.27 million people worldwide die from infections resistant to antibiotics.
- Current tests take 2-5 days to isolate infecting bacteria and identify effective antibiotics.
- In serious infection, every hour without effective antibiotics increases risk of death by 6.7%.
- WA company Cytophenix Pty Ltd to develop antimicrobial susceptibility test that delivers results in less than 5 hours.
UWA Forrest Prospect Fellow Dr Kieran Mulroney at the Harry Perkins Institute of Medical Research has been selected to join Australia’s national biotech incubator – CUREator, which will assist in commercialising the breakthrough technology.
The commercial acceleration incubator that specialises in health security is funded by the federal government via the CSIRO and administered by Brandon BioCatalyst. The incubator is designed to take promising medtech discoveries through early development to commercialisation.
Newly formed Western Australian company, Cytophenix Pty Ltd, a partnership between the researchers, The University of Western Australia and a local AI firm Three Springs Technology, will develop the technology.
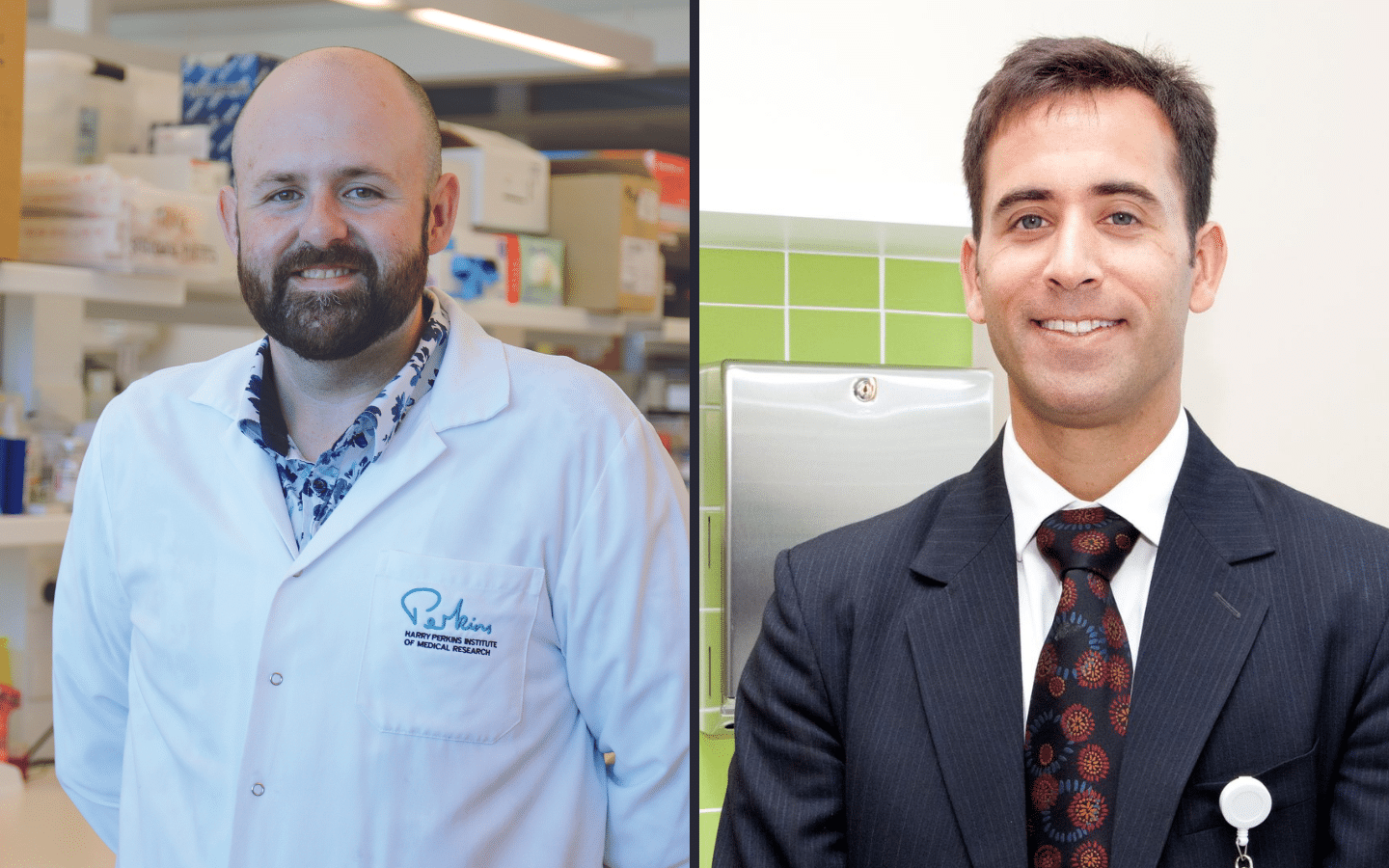
Dr Mulroney (pictured above, left), who led the research team at the Harry Perkins Institute of Medical Research, said the $500,000 commercialisation accelerator grant was an important milestone on the path to bringing the technology to clinical use.
“As a scientist this discovery has been exciting but to see it being translated for the benefit of patients, hopefully in the next five years, is deeply rewarding,” Dr Mulroney said.
“This grant will allow us to accelerate the commercial development technology. It was invented in Western Australia, and this support for our team helps us keep the future commercialisation in WA”, he said.
The technology has been peer reviewed and was published in the international medical journal The Lancet eBiomedicine in July 2022.
“Our technology, the flow cytometry-assisted antimicrobial susceptibility test (FAST), is a rapid and accurate test that returns answers on the best antibiotic to prescribe in just 3-5 hours.
“FAST is a ‘one-principle-fits-all’ platform, meaning it is applicable to essentially all combinations of bacteria, fungi, and the antibiotics that treat them. This includes novel and emerging pathogens,” he said.
Using a device that measures hundreds of thousands of individual bacteria in just a few seconds, the technology detects the damage antibiotics cause to bacteria, and then uses this information to confirm which antibiotic will be an effective treatment.
Across more than 19,000 individual test results from clinical samples, the technology has demonstrated the levels of real-world accuracy and precision required by regulatory agencies for clinical use.
“We can predict which antibiotics will be effective to treat that infection with 96.9 per cent accuracy,” Dr Mulroney said.
Invasive infections with bacteria or fungi are a major cause of death in children and adults worldwide. Without effective antibiotics, patients deteriorate rapidly and can die within hours.
Perth physician, Dr Aron Chakera (pictured above, right) said, “As a renal physician I treat patients with infections that can be life threatening, if the correct treatment is not given as quickly as possible.
“Patients with serious infections cannot survive the several days it can take to return traditional antibiotic test results. Consequently, a broad spectrum, ‘one-size-fits-all’, antibiotic is typically prescribed.
“The biggest problem with prescribing broad-spectrum antibiotics is that it encourages some bacteria to become resistant to the antibiotics. This is a growing and serious problem world-wide.
“The overuse of broad-spectrum antibiotics is one of the key drivers in the spread of resistance to antibiotics.
“In the worst-case scenario we find out several days down the track that we have not been providing effective treatment due to resistance to our first approach.
“This new test would give confidence to patients and their treating doctors”, Dr Chakera said.
For a patient with sepsis, current tests need to grow the bacteria in a blood sample, and then subject them to a lengthy process of additional tests. This can take days to complete, and often results arrive too late to guide the choice of antibiotics used.
Across Europe, the US and Australia approximately 29 million blood cultures are performed annually, representing a market size of $850 million to $1.69 billion AUD.
FAST has been developed in affiliation with PathWest Laboratory Medicine WA and the WA Country Health Service.
The technology will particularly benefit rural and remote patients where access to early diagnosis of sepsis is often difficult.
ENDS
