Predicting relapse for one of the world’s deadliest cancers.
Perth cancer researchers are on track to improve the outcomes of patients with the most common type of primary liver cancer.
Hepatocellular carcinoma (HCC) is one of the most aggressive cancer types. Patients typically suffer a high rate of treatment failures.
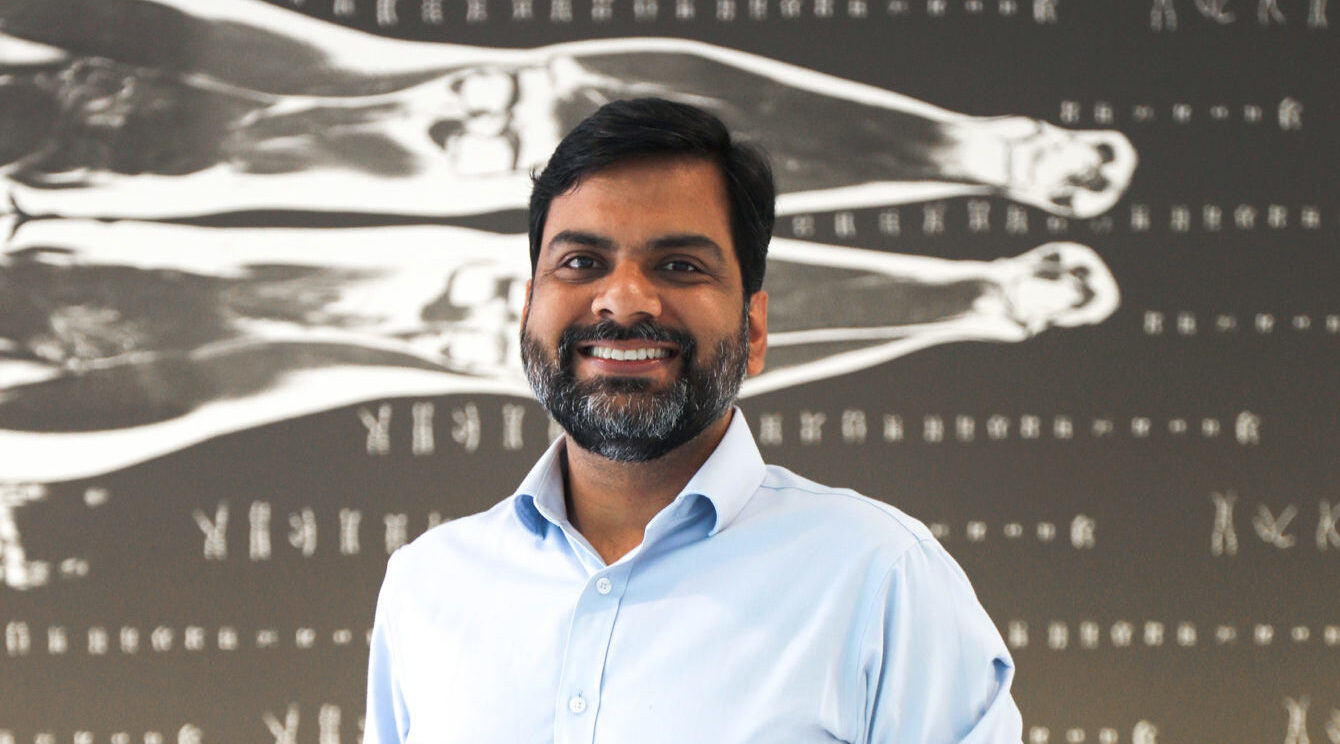
Perth cancer researcher Dr Ankur Sharma (pictured, above) said the key to better outcomes is early detection of new tumours and subsequent treatment response.
“For the 43% of people who are diagnosed with liver cancer at an early stage, the 5-year survival rate is 35% but if the cancer has spread to surrounding tissues or organs and or to the regional lymph nodes, the 5-year survival rate is only 12%.
“We are working on a new blood test to detect the spread of liver cancer before it’s too late,” he said.
Dr. Sharma, who has established a world-leading genomics research laboratory at the Harry Perkins Institute of Medical Research, said approximately 30-50% of patients relapse within two years.
Liver cancer is one of the few cancers on the rise worldwide. The number of new cases per year is predicted to increase by 55.0% between 2020 and 2040.
Smoking cigarettes, drinking alcohol, scarring of the liver which can be caused by hepatitis and alcohol use, can all cause liver cancer.
While surgery and ablation, which is a treatment that destroys liver tumours without removing them, currently represents the most effective treatment approaches for early-stage HCC, long-term survival is hindered by high relapse rates.
“Using sophisticated spatial genomics, (a new frontier in molecular biology that analyses genomic information of single cells), MRI imaging and machine learning algorithms this research will detect changes in millions of tumour cells. Early signs of relapse will then inform treatment response. This combination of latest technology enables the development of a world first software diagnostic package, TRACKERx-ML.
This spatial transcriptomics image shows individual cells in liver cancer tissue and tug of war between immune cells (yellow) and liver cancer cells (turquoise). This project will generate 100’s of such profiles from liver cancer patients to track high risk patients and thereby reduce the relapse rate in HCC.
“With this week’s announcement of $2.5million in funding we will be accessing patient tissue from biobanks around the world including from London, New Delhi, Singapore, Sydney and Perth’s Liver Cancer Collaborative which is supported by the WA Health Department, the Minderoo and McCusker Foundations, UWA, Curtin University and the Harry Perkins Institute.
“We are working to make the product commercially viable. This funding will allow us to develop one of the first blood-based molecular tests to detect relapse in HCC and guide oncologists in patient treatment decisions,” he said.
Dr Sharma anticipates the new test will be available for use in the next 4-5 years.
The research has received $1m funding from the Federal government’s Medical Research Future Fund and matching $1.5m co-funding from Curtin University, the Liver Cancer Collaborative, BGI-Australia and the Harry Perkins Institute of Medical Research.

Michael Twycross is undergoing a liver cancer treatment trial using this latest innovation.
Patient story:
Michael Twycross, a 56-year-old small business owner from Blacktown in Sydney, was diagnosed with liver cancer in late 2021, during the COVID pandemic, following a routine blood test from his GP that saved his life.
Once he was finally referred to a specialist amid the delays caused by COVID, his tumour was removed immediately and he was advised that he was at a high risk of the cancer returning.
Since February 2022, Mr Twycross has been taking part in a trial for a new immunotherapy boosting drug that enables him to be monitored more frequently than most liver cancer survivors, but he admits the threat of the cancer returning is never far from his thoughts.
“It’s like a dark cloud that hangs behind you permanently and you never know when the lightning is going to strike,” Mr Twycross said.
“For me, any initial testing that they can do to find a recurrence early would be an absolute godsend – it would be the best thing ever. Let’s not wait until there’s a giant tumour that we have to address – let’s have a look at a couple of cells that we can hopefully step on quickly, cheaply and without too many side effects. It’s a fantastic idea.
“And if it is to return and they could pick it up early enough, it would be better to treat that patient while they’re still fit and healthy than wait until they are suffering the effects of cancer and then try to treat it when you’re weaker and not able to recover so well.
“Some treatments may even be taken off the table if you wait too long. It just all makes perfect sense.
“If you could have something to tell you as soon as possible, as soon as it could be detected, it would not only give the patient invaluable notice of what’s coming but could also give the clinicians potentially more treatment options. That, coupled with huge potential savings to the government in treating costs, turns this into a technology, where all involved could benefit greatly. In my opinion, the sooner it’s available, the better.”