Researchers from the Western Australia Melanoma Initiative (WAMI), a cancer research collaborative, will implement a specialised immune cell therapy for cancer patients in WA, thanks to a $2.5 million grant from the Cancer Research Trust.
Cellular immunotherapy using tumour-infiltrating lymphocytes (TILs) is a personalised immunotherapy for advanced solid cancers like metastatic melanoma. It is not currently available in Australia. TILs are emerging as an important biomarker in predicting the efficacy and outcome of treatment.
WAMI’s goal to implement TIL therapy has been made possible with the $2.5 million Cancer Research Trust (CRT) grant, and an additional $1 million from the Harry Perkins Institute of Medical Research (Perkins), Edith Cowan University (ECU), the Wind Over Water Foundation, the Spinnaker Health Research Foundation and Cancer Council WA.
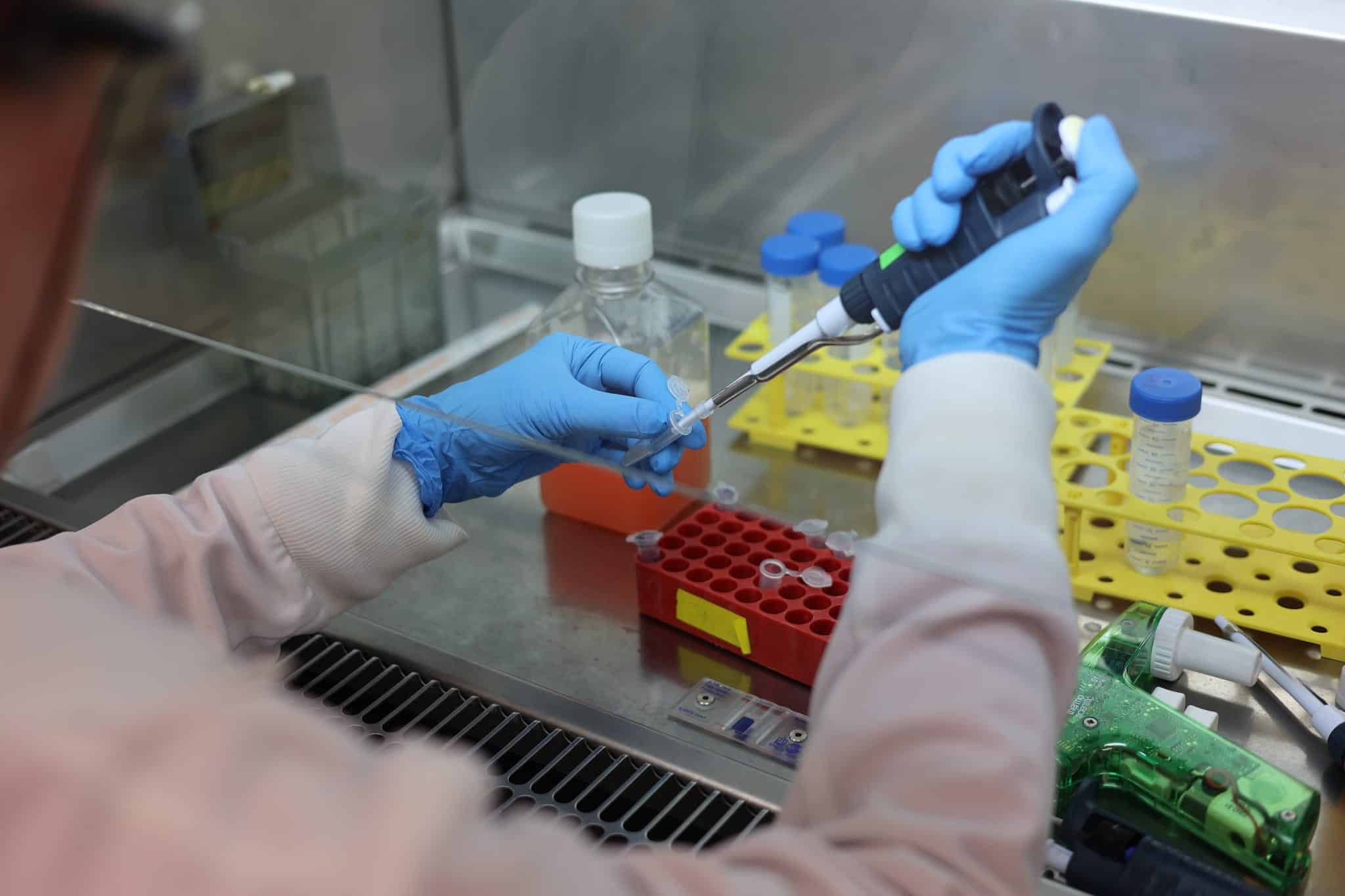
Funding will be used to establish immunotherapy manufacturing infrastructure in WA, improve on existing immunotherapies being used in other countries, and to develop a method using biomarkers to identify patients who are less likely to respond to standard of care treatments and would potentially benefit from TIL therapy.
Each year 17,000 Australians are diagnosed with melanoma, and more than 1300 people die from this disease. 2022 was the first year the number of patients dying of metastatic melanoma decreased, largely because of immunotherapy, where the body’s own immune system is harnessed to treat the cancer. Despite these successes, 50 per cent of all patients with metastatic melanoma still progress in their disease and have limited treatment options.
TIL therapy has yet to be implemented in Australia for patients with melanoma because it is technically challenging, requires access to specialised knowledge and facilities and is time-consuming and expensive.
Chair of Melanoma Discovery at the Harry Perkins Institute, Professor Jonas Nilsson from The University of Western Australia, and Deputy Director of the Centre for Precision Health at ECU Associate Professor Elin Gray, have the knowledge required to implement TIL therapy and identify patients who would need this treatment.
Associate Professor Gray said the team was grateful to the CRT for its grant and for additional funding, including generous donations from families affected by melanoma.
“With this significant investment we will be able to lead the implementation of TIL therapy and identify new ways to improve it. Our hope is that we will be able to work with other centres around Australia and the world to improve patient outcomes for diagnoses other than melanoma, too,” she said.
Professor Nilsson said the ongoing research will be a multidisciplinary effort requiring clinicians, basic researchers and applied cell biologists to provide and improve TIL and other cell therapies.
Dr Peter Lau who is a specialist medical oncologist and a scientist at the Perkins, will help lead clinical implementation of cell therapy in melanoma. “Together with medical oncologists and surgeons, I look forward to reinforcing our multidisciplinary cross-institutional links to bring this personalised treatment to patients,” Dr Lau said.
Professor Nilsson explained further, “We will establish a platform of collaboration where early ideas can be realised, tested in advanced models and translated into clinical practice. We are truly lucky to have access to a TGA-accredited clean room facility that can manufacture cell therapies for patients locally.”
Associate Professor Elin Gray said biomarkers are important to monitor treatment responses and to predict which patients may need new therapies after traditional treatment failure.
“We are confident we can already predict who might respond to standard of care immunotherapy, but we need to implement this technology. Having a therapy to offer these patients makes predictive biomarkers very powerful.”
“In the last year we have developed clinical infrastructure and an analysis platform that extracts much more information from a patient’s blood than is usually analysed in the clinic. This data will be highly useful to alert the cell therapy manufacturing team that there will be a patient needing their therapy,” she adds.
The CRT grant will also support development of new therapies which are based on experiments in advanced models and genomics. A biobank of melanoma biopsies from patients in WA has been established at the Perkins by Jonas and Lisa Nilsson over the last two years and will be used to develop therapy models.
“TIL therapy will be very effective in some patients but not in others since the immune cells may not persist long enough to do their job. Researchers, including Associate Professor Jason Waithman in our collaborative, have preliminary data on how to improve persistence and make the TIL immune cells behave more like stem cells. These data need to be corroborated in models made from specimens from our biobank and have the potential to be a cell therapy for the future,” Professor Nilsson said.
